Tarzana Treatment Centers (TTC) is one of Los Angeles County’s most comprehensive integrated care organizations, providing primary care, behavioral health, substance use disorder treatment, care management, and specialty services with more than 1,400 staff in over 20 locations. With multiple electronic health record (EHR) systems in use and ambitious quality goals, TTC needed a new, reliable way to access timely, complete healthcare and behavioral health information across various hospitals,emergency departments, and partner clinics, particularly for patients with complex care needs.

Evaluating How SUD Treatment Influences ED Use
As one of its quality improvement goals, TTC sought to understand how its substance use disorder (SUD) inpatient treatment impacted the healthcare needs of its patients, particularly those facing homelessness or housing instability. According to a paper published by TTC at the 2025 California Society of Addiction Medicine Annual Conference, individuals with SUD often have high rates of emergency department (ED) utilization due to co-occurring conditions, lack of continuity in care, and unmet treatment needs. And, according to a recent Substance Abuse and Mental Health Services Administration (SAMHSA) report, the number of these substance-related ED visits is steadily rising nationally. While inpatient SUD treatment programs help stabilize patients and connect them to long-term services, their impact on ED utilization patterns remains understudied—yet could have an outsized impact on bending the overall cost of healthcare.
TTC set out to evaluate whether its inpatient SUD treatment reduces ED utilization among those facing homelessness or housing instability by comparing six months post-treatment to six months pre-treatment while accounting for health disparities. But in order to gain access to the comprehensive information leading to accurate insights, TTC knew it needed to be able to access and consolidate both behavioral health and healthcare information from patients visiting a variety of providers across California.
Challenges Within TTC’s Existing Infrastructure
TTC’s existing systems and processes presented numerous challenges to this goal, including:
- Access to information contained within various EHRs, which was largely siloed
- Large gaps in visibility into patient care events
- Delays in information, which resulted in delayed follow-up, which negatively impacted coordination and continuity
- A limited ability to analyze population insights comprehensively
- Missing histories for patients, especially those receiving behavioral health support

To solve these issues, TTC sought a platform that would reach across disparate systems and care providers to deliver a consolidated, accurate, and complete view into patients by drawing on both health and behavioral health information.
A QHIO Partner Capable of True Data Integration
After evaluating California’s QHIOs, TTC selected the LANES platform for its broad and deep provider and patient reach and for its ability to deliver a complete, accurate, and integrated view into health care and behavioral health information. With behavioral health information integration, a historically common systemic issue due to stringent privacy and security requirements, LANES uniquely manages both types of information in order to give entities like TTC the tools they need to deliver comprehensive care for its patients, meet quality goals, and improve overall patient outcomes.
Key LANES functionality used included:
- Real-time hospital & emergency department ADT alerts
- Clinical document exchange from all hospitals and health systems, not just those using the same EHRs as TTC
- Consolidated patient clinical timelines
- Cross-system medication and history review
- Data extraction for population-level QI analysis
When TTC was preparing its study to examine the impact of its inpatient treatment programs, it enlisted the LANES platform. With the help of LANES’ complete and robust patient healthcare and behavioral health information, TTC gained real-time visibility into patient information, no matter which provider they visited and which EHR their information was recorded in. As a result, TTC could examine how patients that had received inpatient care used healthcare services, specifically ED use, to manage their care needs before and patient inpatient programs were utilized.
The Power of Integrated Behavioral and Medical Data
By integrating clinical and social data from multiple systems, LANES enabled TTC to accurately track patient outcomes. The findings revealed that patients that went through TTC’s inpatient SUD programs experienced a dramatic decline in unnecessary ED visits post-treatment. On average, visits declined from 2.6 to 0.4 in those six months after treatment.
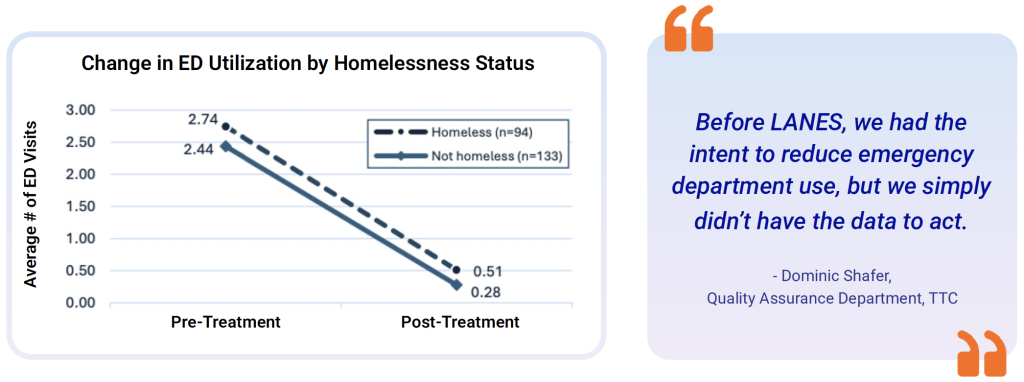
These insights and outcomes not only inform TTC’s own quality goals and future efforts, but also serve as a model for access to SUD inpatient programs in California and across the nation while also opening up additional opportunities to explore how to drive better, more efficient outcomes. TTC is now focused on a multi-year effort to reduce avoidable ED visits and hospital admissions, using LANES data to monitor progress and guide workflow design.

